THE MANY FACES AND CAUSES OF SCIATICA

Sciatica merely describes a path of pain and is not a specific diagnosis. The use of the term "sciatica" does not specify a cause.
Defined, "sciatica" is a description of a particular path of pain following the sciatic nerve as it traverses the buttock (hip) and/or continues down the back of the thigh, outside of the leg and perhaps the foot. As our article title denotes, sciatica can be a real pain in the buttocks.
Generally, the worse the condition, the further down the leg the pain travels and may even affect the foot. However, there are certain cases that although severe, only affect the hip area or buttock. It suffices to say that the symptom picture can be quite varied from one individual to another. Although most commonly associated with nerve compression from a low back disc condition, there are many causes of sciatica, some of which are not back related. Interestingly enough even those cases originating from a low back condition may not exhibit any back pain.
Some authorities would argue that if the origin of pain is not compression of a nerve root in the lower back, the result is not a "true sciatica", but a
pseudo-sciatica. Synonyms for sciatica would be
sciatic neuralgia or
sciatic neuritis.
ANATOMY OF THE SCIATIC NERVE

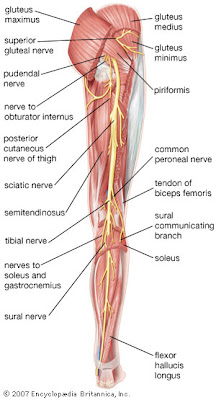
The
sciatic nerve is about 1/2 inch in diameter and is known to be the longest and largest nerve in the human body. The nerve originates in the lower spine as nerve roots exit the spinal cord (between the vertebrae in the spine), and combine to extend all the way down the back of the leg to the toes.
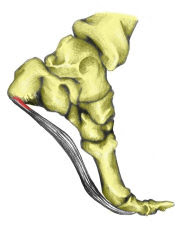
It is thus composed from a combination of 5 nerve roots exiting holes known as foraminal openings between vertebrae in the lower lumbar and sacral region. These include the following nerve roots: L4, L5, S1, S2, and S3. Nerve roots in the lumbo-sacral area of the spine are named by the vertebrae above. Thus if the nerve root exits between L5 and S1 it would be considered the L5 nerve root. By understanding this one can correlate the area of symptoms with a specific spinal level.
The five nerves combine anterior to (in front of) the piriformis muscle to become the sciatic nerve. This nerve then travels down the back of each leg, branching out to innervate specific regions of the leg and foot. It should be mentioned here that a spasm of this piriformis muscle where the nerve crosses the sciatic notch can cause sciatic neuralgia and often mimic sym
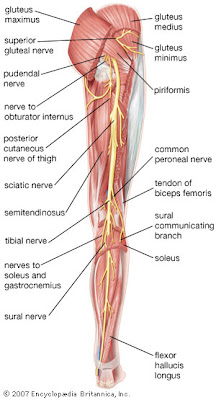
ptoms of a herniated lumbar disc.
Just above the back of the knee, the sciatic nerve divides into two nerves, known as the peroneal and tibial nerves, going to various parts of the lower leg:
- The peroneal nerve innervates the shin and outer aspect of the leg down to the upper foot.
- The tibial nerves innervates the posterior portion of the leg and traverses all the way to the feet to innervate both the heel and sole of the foot.
The sciatic nerve supplies both motor input (eliciting muscle movement and reflexes) as well as sensory innervation.
SYMPTOM PICTURE OF SCIATICA
Pain: searing , stabbing, usually intermittent pain is generally the overwhelming symptom. The pain can be felt in the low back, buttock, posterior and outer side of the thigh or leg and possibly all the way to the toes. The pain is most often felt in certain positions, while walking or while straightening the leg. It may occur on both sides (bilaterally), but it is more often one-sided (unilateral). Pain is sometimes exacerbated by sneezing, coughing, laughing or pushing during a bowel movement (Valsalva's Maneuver).
Numbness/tingling: sometimes the pain is either accompanied by or replaced by numbness and tingling known as paresthesia or radiculopathy.
Weakness: in the most severe cases of sciatica there is actually impairment of the motor nerve functions causing weakness in the leg and/or foot. The most common sign of such would be foot drop or the inability to pull the big toe up toward your knee (aka: lack of dorsiflexion).
CATEGORIES OF CAUSES
Mechanical Spinal Nerve Compression: most often from a herniated, ruptured or extruded disc but can be from severe misalignment or vertebral subluxation.
Compression by Muscle Spasm: most commonly known as a "Piriformis Syndrome" whereby the muscle underlying the gluteus maximus (buttock) is spasmed applying pressure to the sciatic nerve underneath. This is known to clued physicians as an "entrapment neuropathy" and is often misdiagnosed as a low back disk herniation because it mimics many of the symptoms of such. This can prudently be differentially diagnosed from a disc herniation by either MRI studies, CT scan or just a good old fashion history and exam including questions regarding pain during coughing, sneezing and bowel movements.
Trauma to the Sciatic Nerve: bruising, puncture wounds, or over-stretching injuries to the nerve itself can produce the symptoms of sciatica.
Spondylolisthesis: this is a slippage of one vertebral body on top of another and may be a result of fracture or a genetic defect in the
pars interarticularis. If in the L4 to S1 region, sciatic neuritis symptoms can occur. Although many authors seem to describe a compression of nerve roots resulting from a spondylo-listhesis, it has been my experience both clinically and in my review of the literature that the most accepted authorities believe the nerve root irritation to be a result of traction or stretch of the nerves vs. an actual compression.
Spinal Tumors: space occupying lesions, of the spinal vertebrae, spinal cord, cauda equina, or surrounding muscles or sciatic nerve itself can cause sciatic symptoms.
Sacro-iliac Joint Sprain or Subluxation: this is actually one of the least understood or recognized conditions causing sciatica, but in this clinician's experience is one of the most common causes of sciatica not resulting in pain extending below the knee. Coughing and sneezing does not increase the symptoms in this case and often Kemp's sign will NOT be positive. Subluxation or sprain of the sacro-iliac joint leads to a referred sciatica in this case. This is generally best treated by a chiropractic physician.
Chemical Irritation: although not even known or considered by most practicing physicians,
chemical radiculalgia is one of the physical results of back dysfunction and can be the primary cause of sciatica. This is an actual irritation to nerve roots caused by the swelling pressure of inflammation against the nerve. It is a major factor in what is called the "cycle of pain". It may be interesting to note that it has been this practitioner's experience that this is often the factor that is most concerning when dealing with the sequela of a disc herniation or injury. It is the overwhelming reason that
Lumbar Epidural Steroid Injections have been so effective in relieving the symptoms of herniated or ruptured disc conditions. It leads some researchers to believe that inflammation may play an even greater roll in symptomatology than the mechanical pressure of displaced disc material.
Viscerally Referred Pain: although not as common as some of the other causes of sciatic symptoms, paresthesias, pain and odd sensations may be felt along the sciatic nerve distribution as a result of problems with internal organs. For example, problems with the prostate gland or female organs can refer sensations along the sciatic nerve. This can easily be ruled out by a thorough examination.
TREATMENT OF SCIATICA
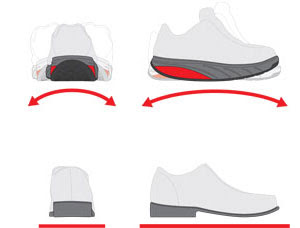
Certainly the best treatment practices for sciatica would include addressing the cause in addition to alleviating the symptoms. Thus the approach may be different dependent on the cause. Sitting, driving and arising from the sitting position is usually a problem for all sciatica sufferers and thus one of the most recommended items would be a pressure relieving seat cushion. One type is known as a
memory foam seat wedge. The 2nd type is a
gel seat cushion that is wedged for ultra comfort. Make sure that the cushion you select has a cut-out for the coccyx or tailbone and that it is solid, fairly dense memory foam or a solid type of gel. Ice is nice in the case of sciatica and heat should generally be avoided in acute cases.
Other treatment protocol is more causal specific and usually requires a battery of prescribed and self-care. Some of these are listed below:
DON'TSAvoid irritation and stretching of the nerve during the healing process. This would eliminate toe touching with the leg straight.
Avoid running, fast walking or other physical activities that increase pain.
Avoid heavy lifting, stooping, squats or prolonged bending.
Avoid sitting on soft overstuffed chairs or couches or desk chairs that fall away when leaned against.
Avoid fast movements.
Avoid arising out of bed w/o first turning on your side
Avoid stomach sleeping or sleeping on your back with both legs straight out.
Avoid straightening the involved leg when sitting.
DO'SDo see a physician or chiropractor for a proper diagnosis and treatment. Depending on findings your doctor of choice may suggest: spinal adjustments or manipulation, deep tissue massage of the buttocks, core muscle strengthening and stretching, repair of a disc herniation, oral anti-inflammatories, lumbar corset or lumbar epidural cortisone injections. Lumbar traction and/or gravity inversion may be advisable in some cases. For less common causes like tumors or referred pain from internal organs, your doctor will likely refer you to a specialist for further investigation.
When sleeping on your back, keep at least the involved leg slightly bent with an
orthopedic bed wedge or soft fluffy pillow.
When side sleeping, place a soft pillow between your legs starting at the knee and positioned downward from there.
Do utilize a memory foam seat wedge to keep good posture and remove pressure from the sciatic nerve when seated or driving. For chronic sciatica seated workers should consider the purchase of a
nimble ergonomic chair like the Bodybilt task chair.

 T functionality could be likened to that of the old Joe Palooka Bob Bag of the 1950's. This was a self-righting punching toy with a counter-weighted bottom. No matter what one did to it, it righted itself in a perfectly vertical format.
T functionality could be likened to that of the old Joe Palooka Bob Bag of the 1950's. This was a self-righting punching toy with a counter-weighted bottom. No matter what one did to it, it righted itself in a perfectly vertical format.